Quick Summary:
Subcutaneous BBL is a safety-focused technique that injects fat exclusively into the layer above the muscle, reducing fatal fat embolism risk. According to ASERF guidelines and autopsy studies, no BBL deaths have occurred when fat remained only in the subcutaneous plane.
The 2022 multi-society safety advisory established subcutaneous-only injection as the standard of care, with Florida becoming the first state to legally mandate ultrasound guidance for all BBL procedures in July 2023.
This guide covers the science behind subcutaneous technique, safety statistics, how ultrasound guidance works, and what patients should know when choosing a surgeon.
Why Trust This Guide
This article draws from peer-reviewed research published in Aesthetic Surgery Journal, ASERF Task Force recommendations, multi-society safety advisories from ASPS/ISAPS/ASAPS, and FDA guidelines. All medical claims are supported by source citations from recognized plastic surgery organizations.
Carely Clinic’s editorial team collaborates with board-certified plastic surgeons to ensure accurate, balanced information that helps patients make informed decisions about body contouring procedures.
What Is Subcutaneous BBL?
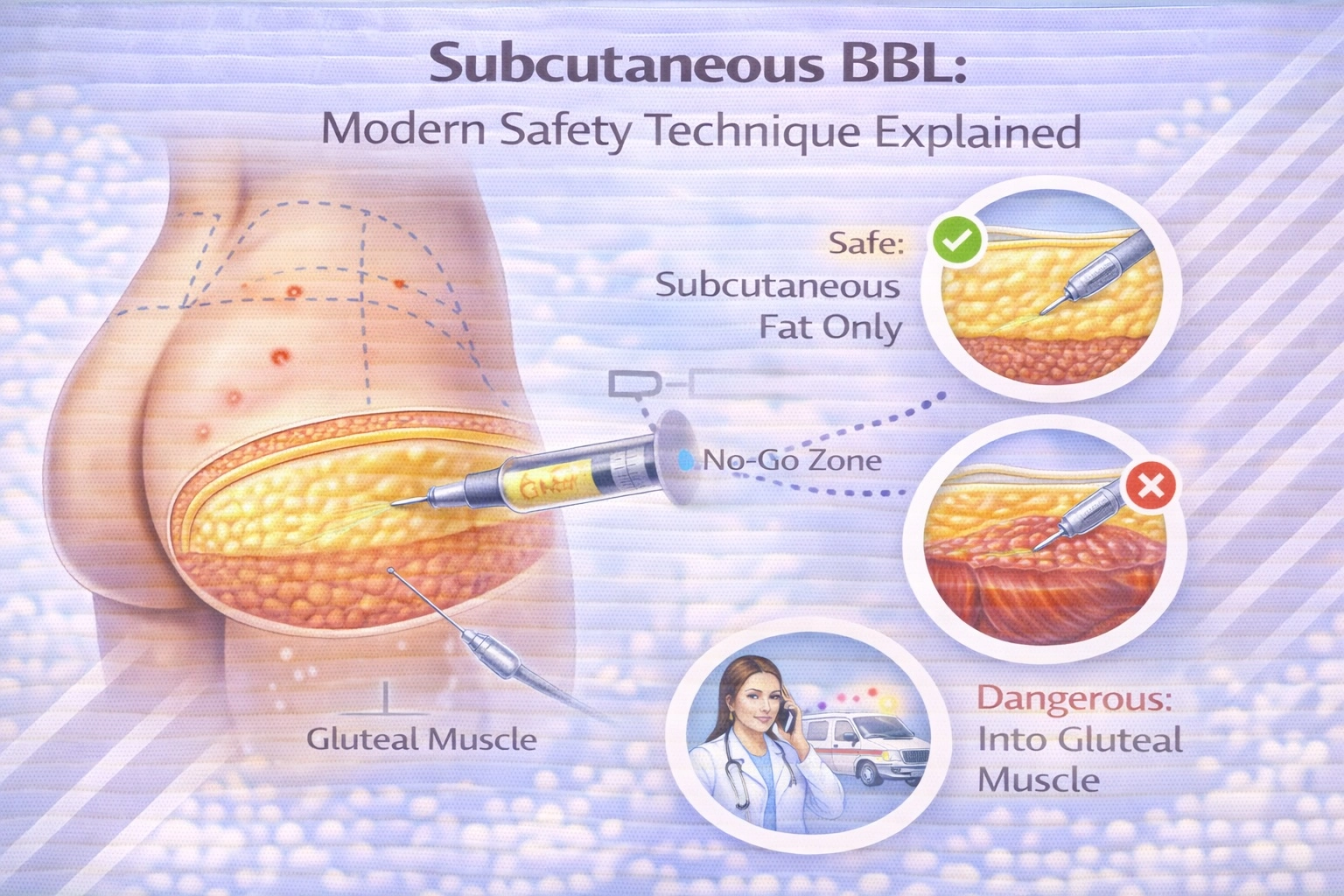
Subcutaneous BBL is a fat grafting technique that injects purified fat exclusively into the tissue layer between the skin and muscle, never crossing into the gluteal muscle or deeper planes. This approach follows 2022 ASERF/ASPS safety guidelines establishing subcutaneous-only injection as the standard of care.
The gluteal region contains distinct anatomical layers. The subcutaneous space sits between the dermis (skin) and the deep gluteal fascia that covers the gluteus maximus muscle. Research published in Aesthetic Surgery Journal identified seven distinct deep subcutaneous fat compartments that can be selectively filled for buttock augmentation while maintaining a safe distance from major blood vessels.
Traditional BBL techniques often involved injecting fat into the gluteal muscle itself, believing this would improve fat survival due to the muscle’s rich blood supply. However, autopsy studies of BBL fatalities revealed that intramuscular injection was directly linked to fatal fat embolism. The subcutaneous technique was developed specifically to eliminate this risk.
The subcutaneous fat layer thickness varies across the buttock, ranging from approximately 1 centimeter at the outer hips to 3-4 centimeters at the central gluteal dome. This creates a curved target that requires precision, which is why ultrasound guidance has become essential for safe subcutaneous BBL procedures.
Why Was This Technique Developed?
The subcutaneous-only technique emerged after alarming mortality rates made BBL the deadliest cosmetic procedure. The 2017 ASERF Task Force reported mortality estimates as high as 1 in 3,000 procedures, prompting urgent investigation into the cause of deaths and development of safer protocols.
Between 2015 and 2018, multiple studies examined BBL fatalities through autopsy reports and case reviews. The consistent finding was devastating in its clarity: in every documented death, fat had been injected into the gluteal muscle. In no case of death had fat been found only in the subcutaneous plane.
This discovery led the Multi-Society Task Force for Safety in Gluteal Fat Grafting—representing ASAPS, ASPS, ISAPS, IFATS, and ISPRES—to issue an urgent warning in 2018. The advisory stated unequivocally that fat should never be placed in the muscle and should only be placed in the subcutaneous tissue.
The plastic surgery community’s response was significant. A 2019 survey showed that the percentage of surgeons injecting exclusively into subcutaneous fat had increased to 85.7%, compared to only 39.8% in 2017. This shift corresponded with improved mortality statistics, demonstrating that technique modification could save lives.
The Science: How Fat Embolism Occurs
Fatal fat embolism occurs when injected fat enters large gluteal veins and travels to the heart and lungs, blocking pulmonary circulation. This happens when the injection cannula damages gluteal veins located within or beneath the muscle, allowing fat to enter the bloodstream under injection pressure.
The gluteal region contains major blood vessels, including the superior and inferior gluteal veins, that drain into the internal iliac vein and ultimately the heart. These vessels are located primarily within the gluteal musculature and in the submuscular space. A 2024 study in Aesthetic Plastic Surgery found that intramuscular vessels have significantly larger caliber than subcutaneous vessels, explaining why muscle injection carries greater risk.
Two mechanisms can cause fat to enter the venous system. The first is direct cannula penetration into a vein, allowing fat to be injected directly into the bloodstream. The second, called the “venous traction theory,” involves fat migrating from a high-pressure extravascular space into a low-pressure venous system through vessel injury.
The submuscular plane beneath the gluteus maximus is particularly dangerous because it’s loose connective tissue. When this space is stretched during fat injection, gluteal veins can tear, creating a siphoning effect that draws fat cells into the circulation. This explains why even experienced surgeons who believed they were above the muscle still experienced patient deaths—the cannula can inadvertently cross into dangerous territory without visual confirmation.
Expert Insight
“In every patient who has died, at autopsy, fat was seen within the gluteal muscle. In no case of death has fat been found only in the subcutaneous plane. The subcutaneous plane has not been linked to pulmonary fat embolism.”
— Multi-Society Task Force for Safety in Gluteal Fat Grafting, 2018 Advisory
Subcutaneous vs Intramuscular Injection
The key difference between subcutaneous and intramuscular BBL is anatomical placement: subcutaneous injects fat above the muscle fascia where no major veins exist, while intramuscular places fat within the muscle where large vessels create embolism risk.
| Factor | Subcutaneous Technique | Intramuscular Technique |
|---|---|---|
| Injection Location | Above deep gluteal fascia, in fat layer | Within gluteus maximus muscle |
| Fat Embolism Risk | Zero documented fatalities when properly executed | Directly linked to all BBL deaths |
| Vessel Exposure | Smaller subcutaneous vessels only | Large gluteal veins present |
| Fat Retention Rate | 64-82% at 12 months (prospective studies) | Similar long-term retention |
| Ultrasound Guidance | Recommended/Required (Florida law) | Not applicable (technique abandoned) |
| Current Status | Standard of care (2022 guidelines) | Abandoned by safety societies |
| Aesthetic Results | Natural contour with proper technique | N/A (no longer recommended) |
A critical misconception was that intramuscular injection provided better fat survival because muscle has superior blood supply. However, a 2019 prospective study published in Plastic and Reconstructive Surgery demonstrated that subcutaneous-only gluteal fat augmentation achieved comparable long-term retention. The study found an average increase in gluteal subcutaneous layer thickness of 56.51% immediately post-operatively, with 81.84% of that gain maintained at 12 months.
The anatomical studies also revealed that fat injected intramuscularly doesn’t stay in place—it migrates through the muscle into the deeper submuscular space where the most dangerous vessels are located. This means there is no “safe zone” for intramuscular injection, contrary to earlier claims in the literature.
Ultrasound-Guided BBL: The Safety Standard
Ultrasound-guided BBL uses real-time imaging to visualize cannula position during fat injection, ensuring fat remains in the subcutaneous layer and never crosses into muscle. This technology has become the gold standard for safe BBL procedures, with Florida mandating its use by law since July 2023.
The technique, sometimes called ultraBBL or ULTRA BBL (Ultrasound-guided Lipofilling Targeting Recipient Areas), was pioneered by Dr. Pat Pazmiño in Miami. The surgeon holds an ultrasound probe against the skin while injecting, creating a live video feed that shows exactly where the cannula tip is located relative to the muscle fascia.
Ultrasound visualization reveals two distinct subcutaneous fascial layers: the deep gluteal fascia covering the muscle surface, and the superficial gluteal fascia lying under the dermis. Between these layers exist the superficial and deep subcutaneous fat compartments—the target zones for safe injection.
The benefits of ultrasound guidance extend beyond safety. Surgeons can identify the seven deep gluteal fat compartments and selectively fill them to achieve specific aesthetic outcomes. The technology allows precise volume placement, improved symmetry, and optimization of fat survival by targeting the most favorable tissue planes.
According to a 2021 study in The American Journal of Cosmetic Surgery, practices using wireless ultrasound-guided gluteal fat grafting reported excellent safety profiles. The Centre for Surgery in London reported over 500 ultrasound-guided BBL procedures since 2019 with no serious complications.
Expert Insight
“ULTRA BBL should be learned by surgeons performing gluteal fat grafting and should be incorporated into their practices. Surgeons not familiar with the techniques of ULTRA BBL should consider attending a technique-related training course.”
— Practice Advisory on Gluteal Fat Grafting, Aesthetic Surgery Journal, 2022
Safety Statistics: What the Research Shows
BBL mortality rates have decreased significantly since the adoption of subcutaneous-only technique, dropping from 1 in 3,000 in 2017 to approximately 1 in 15,000-20,000 in recent surveys—making it comparable to other major cosmetic procedures like abdominoplasty.
The evolution of BBL safety statistics tells an important story. The initial 2017 ASERF survey reported a mortality rate of 1 in 3,448, which was later recalculated by Del Vecchio et al. to approximately 1 in 13,000. A 2019 follow-up survey, conducted after widespread adoption of safety recommendations, found the fatality rate had improved to 1 in 14,952.
A 2024 study of American Board of Cosmetic Surgery (ABCS) surgeons showed even more encouraging results. Among 12,172 gluteal fat grafting cases performed between 2019-2021 by surgeons following current safety recommendations, there were zero fatal and zero non-fatal pulmonary fat embolisms reported. Notably, 82 of 85 participating surgeons reported injecting fat “exclusively” above the muscle.
However, context matters. The South Florida experience demonstrates that technique guidelines alone are insufficient without enforcement. Between 2010 and 2022, South Florida experienced 25 BBL-related fat embolism deaths, with 14 occurring after the ASERF guidelines and Florida Board of Medicine’s “subcutaneous-only” rule were implemented. The majority of deaths (92%) occurred at high-volume, budget clinics where proper protocols weren’t consistently followed.
This data underscores a critical point: subcutaneous BBL is safe when performed correctly by trained surgeons using proper visualization, but the technique’s safety depends entirely on execution. This is why regulatory measures like Florida’s ultrasound mandate became necessary.
The 2022 Multi-Society Safety Guidelines
The April 2022 Practice Advisory on Gluteal Fat Grafting established comprehensive safety protocols endorsed by ASPS, ASAPS, and ISAPS, codifying subcutaneous-only injection, ultrasound guidance, and operational safeguards as the standard of care.
The 10 main principles from the 2022 advisory include:
Technical Requirements:
- Fat must be placed exclusively in the subcutaneous plane
- Ultrasound guidance should be used to confirm and document the layer of fat placement
- Cannulas should be 4mm or greater in diameter for fat insertion
- Avoid Luer-Lock syringes; use roller pump techniques for volumes exceeding 200mL per buttock
Operational Safeguards:
- Minimize distraction and operator fatigue during fat transplantation
- Utilize a “single-surgeon” approach—one surgeon performs the entire procedure
- Perform no more than 3 gluteal fat grafting cases per surgeon per day
- The surgeon cannot delegate critical portions of the procedure to assistants
Documentation and Oversight:
- Maintain ultrasound video recordings with time and date stamps
- Establish proper doctor-patient relationships before surgery day
- Active pre-operative and post-operative engagement with patients
The advisory also addressed emerging technologies. While ultrasound guidance is the current standard, the societies acknowledged that equivalent or superior imaging technologies may be authorized by medical boards as they become available. The key requirement is real-time visualization confirming subcutaneous placement.
Florida’s BBL Law: A Legal Precedent
Florida’s HB 1471, effective July 1, 2023, became the first law in the United States to mandate ultrasound guidance during BBL procedures, establishing legal requirements that may influence standards nationwide.
The law was passed following a public health emergency declaration by the Florida Board of Medicine in June 2022, when 2021 became the deadliest year for BBL surgery in the state with eight women dying from fat embolism in South Florida alone. The emergency rule that preceded the law limited surgeons to three BBL procedures per day and required ultrasound guidance during injection.
Key provisions of HB 1471 include:
Mandatory Ultrasound Guidance: Physicians must use ultrasound (or equivalent board-authorized technology) to ensure fat is injected only into the subcutaneous space, not crossing the fascia overlying the muscle.
Documentation Requirements: Surgeons must maintain ultrasound video recordings in the patient’s medical record with time and date stamps, providing evidence of proper technique.
Patient Safety Protocols: Surgeons cannot meet patients for the first time on surgery day—an in-person examination must occur at least one day before the procedure.
Delegation Prohibition: Both fat extraction and fat injection must be performed by the physician and cannot be delegated to nurses or assistants.
Procedural Limits: Physicians may only perform one gluteal fat grafting procedure at a time, with a one-to-one patient-to-physician ratio in the office.
The law also introduced financial accountability, with fines of $5,000 per incident for violations. Additionally, a 2024 update (HB 1561) set new liability coverage requirements for surgeons performing liposuction and BBL procedures.
The Florida Society of Plastic Surgeons praised the legislation, with Dr. Pat Pazmiño stating that it marked the first time a plastic surgery law had passed in the state, making ultrasound “the law of the land” for BBLs.
How This Applies in Turkey
International guidelines from ASPS, ISAPS, and ASERF apply equally at Turkey’s JCI-accredited medical facilities. Turkish hospitals performing subcutaneous BBL follow identical clinical protocols and safety standards as American and European institutions.
The key differences between Turkey and Western countries are cost and accessibility. BBL in Turkey costs €3,300-€5,500 all-inclusive compared to $8,000-$20,000 in the USA and £6,000-£15,000 in the UK, representing 60-75% savings. International patients typically complete the entire consultation-to-recovery process within 7-10 days, compared to weeks or months of waiting in countries with longer surgical scheduling.
Turkey has become one of the top destinations for international cosmetic surgery, according to ISAPS 2024 data. The country’s high surgical volumes mean experienced surgeons perform significantly more BBL procedures annually than their Western counterparts, developing specialized expertise in body contouring.
At Carely Clinic in Istanbul, BBL is performed by board-certified plastic surgeons at JCI-accredited partner hospitals using subcutaneous technique with ultrasound guidance. Packages include pre-operative testing, surgical fees, anesthesia, hospital stay, 5-star hotel accommodation, private transfers, compression garments, and lifetime support.
Learn more about Brazilian Butt Lift at Carely Clinic.
What to Ask Your Surgeon
Before undergoing BBL, patients should verify their surgeon uses subcutaneous-only technique with ultrasound guidance and follows current multi-society safety guidelines. The questions below help ensure you’re choosing a qualified, safety-conscious provider.
Essential Questions to Ask:
- “Do you inject fat exclusively into the subcutaneous layer, above the muscle?”
- The answer should be an unequivocal yes. Any surgeon still performing intramuscular injection is not following current safety standards.
- “Do you use ultrasound guidance during fat injection?”
- Real-time visualization is now considered essential for confirming proper placement. Ask to see the ultrasound equipment they use.
- “How many BBL procedures do you perform per day?”
- Guidelines recommend no more than 3 per day per surgeon to prevent fatigue-related errors.
- “Will you personally perform the entire procedure, or will assistants inject fat?”
- The surgeon should perform all critical portions—delegation to assistants has been linked to complications.
- “What is your complication rate, specifically for fat embolism?”
- Experienced surgeons using proper technique should have zero fat embolism incidents.
- “Are you board-certified in plastic surgery, and are you a member of ISAPS, ASPS, or equivalent society?”
- Board certification and professional society membership indicate training and commitment to safety standards.
- “Will you provide ultrasound video documentation of my procedure?”
- Documentation protects both patient and surgeon by proving proper technique was used.
Red Flags to Avoid:
- Surgeons who dismiss ultrasound guidance as unnecessary
- Facilities performing more than 3-5 BBLs per day per surgeon
- Meeting the surgeon for the first time on surgery day
- Quotes significantly below market rate (suggests corner-cutting)
- Inability to provide credentials or patient testimonials
Summary Table: Technique Comparison
| Safety Factor | Traditional BBL (Pre-2018) | Subcutaneous BBL (Current Standard) |
|---|---|---|
| Injection Plane | Intramuscular or mixed | Subcutaneous only (above fascia) |
| Visualization | Blind injection (tactile only) | Ultrasound-guided real-time imaging |
| Mortality Rate | ~1 in 3,000 (2017 data) | ~1 in 15,000-20,000 (current data) |
| Fat Embolism Risk | Significant (all deaths linked) | Minimal (zero deaths when properly executed) |
| Guideline Status | Abandoned by major societies | Standard of care (2022 Advisory) |
| Legal Requirements | N/A | Mandated in Florida (HB 1471) |
| Documentation | Standard surgical notes | Ultrasound video with timestamps |
| Surgeon Limits | No restrictions | ≤3 procedures per day recommended |
| Fat Retention | Variable (60-80%) | Comparable (64-82% at 12 months) |
| Turkey Cost | N/A | €3,300-€5,500 all-inclusive |
| USA Cost | N/A | $8,000-$20,000+ (surgery only) |
Frequently Asked Questions
What exactly is subcutaneous BBL?
Subcutaneous BBL injects fat only into the tissue layer between skin and muscle, never crossing the deep gluteal fascia. This technique eliminates fat embolism risk by avoiding the large gluteal veins located within the muscle. All major plastic surgery societies now recommend this as the exclusive injection method following 2022 multi-society guidelines.
Why is subcutaneous technique safer than traditional BBL?
Autopsy studies show 100% of BBL deaths involved fat in the muscle layer, while zero deaths occurred with subcutaneous-only placement. The muscle contains large gluteal veins that, when injured, allow fat to enter the bloodstream and travel to the lungs. Subcutaneous tissue has only small vessels that cannot accommodate fat particles large enough to cause fatal embolism.
Is ultrasound-guided BBL mandatory?
Ultrasound guidance is legally mandatory in Florida since July 2023 under HB 1471. All major plastic surgery societies recommend it as standard practice worldwide. The technology allows surgeons to confirm real-time cannula position and document that fat remains in the subcutaneous plane. While not legally required outside Florida, it represents the current standard of care.
How much does subcutaneous BBL cost?
Subcutaneous BBL costs $8,000-$20,000 in the USA (surgery fees only), £6,000-£15,000 in the UK, and €3,300-€5,500 in Turkey for all-inclusive packages. Turkey prices include surgeon fees, hospital stay, accommodation, transfers, and follow-up care at JCI-accredited facilities. The 60-75% savings reflect lower operational costs, not lower quality or safety standards.
What is the mortality rate for subcutaneous BBL?
The mortality rate is approximately 1 in 15,000-20,000 procedures when surgeons follow current safety protocols, down from 1 in 3,000 in 2017. A 2024 ABCS study of 12,172 cases using subcutaneous-only technique reported zero fatal fat embolisms. Proper execution with ultrasound guidance effectively eliminates this risk according to multi-society safety data.
How long do subcutaneous BBL results last?
Results are permanent after fat cells establish blood supply at 3-6 months post-procedure. Prospective studies show 64-82% of transferred fat survives at 12 months, with an average 18% reabsorption from immediate post-operative measurements. Surviving fat behaves like natural fat, so weight gain or loss will affect results proportionally over time.
Can I get good results with subcutaneous technique only?
Yes, cadaveric studies identified seven distinct deep subcutaneous fat compartments that provide projection and volume. Surgeons using ultrasound guidance can selectively fill these compartments to achieve natural contours comparable to or better than intramuscular injection. The technique limitation is anatomical space, not aesthetic potential, requiring realistic volume expectations based on existing subcutaneous thickness.
What are the main risks of subcutaneous BBL?
Common risks include swelling, bruising, temporary numbness, and asymmetry affecting most patients. Serious complications include infection (1-3% of cases), seroma, fat necrosis, and skin irregularities. Fat embolism risk drops to near-zero with proper subcutaneous technique. Approximately 15-35% of patients experience some fat reabsorption requiring potential touch-up procedures.
How can I verify my surgeon uses subcutaneous technique?
Ask if they inject exclusively above the muscle fascia and use ultrasound guidance throughout injection. Request to see their ultrasound equipment and ask for video documentation protocols. Inquire about their complication rates, specifically fat embolism incidents (should be zero). Board-certified surgeons following 2022 guidelines will answer these questions directly and show their safety protocols.
Is BBL in Turkey as safe as in the USA?
Safety depends on surgeon technique and facility standards, not geography. JCI-accredited Turkish hospitals follow identical international protocols as US facilities. Key verification points are surgeon board certification, ultrasound guidance use, subcutaneous-only technique, and proper patient limits. Turkish surgeons often perform higher case volumes, building specialized expertise in body contouring procedures.
Does insurance cover subcutaneous BBL?
No, BBL is considered cosmetic and not covered by health insurance in the USA, UK, Turkey, or most countries. Patients pay out-of-pocket or use medical financing options. Some exceptions exist for reconstructive cases following trauma, cancer surgery, or congenital deformities, requiring medical necessity documentation and prior authorization from insurance providers.
What happens if fat is accidentally injected into muscle?
Intramuscular injection creates immediate risk of fat entering large gluteal veins through vessel injury or pressure differential. If fat reaches the bloodstream, it travels to the heart and lungs, potentially causing pulmonary fat embolism with symptoms including chest pain, breathing difficulty, and rapid heart rate within minutes to hours. This is a medical emergency requiring immediate intensive care.
Conclusion
Subcutaneous BBL represents a fundamental advancement in patient safety, directly addressing the mechanism that caused BBL’s dangerous reputation. The science is clear: when fat remains above the muscle fascia, the risk of fatal fat embolism drops to effectively zero.
The combination of subcutaneous-only technique with ultrasound guidance has transformed BBL from “the deadliest cosmetic procedure” to one with safety statistics comparable to common surgeries like abdominoplasty. However, this safety depends entirely on surgeon compliance with established protocols.
For patients considering BBL, the priority should be verifying your surgeon uses current safety standards—subcutaneous injection with ultrasound guidance, proper case limits, and full surgeon involvement. Price should be a secondary consideration after safety verification.
Individual requirements and outcomes vary. This guide provides general information based on international medical guidelines. Consult qualified medical professionals for personalized advice.
For more information about subcutaneous BBL at Carely Clinic, request a consultation or explore our BBL Turkey pagefor complete package details.
Medical Review: Dr. Aliraz Jahangirov