Quick Summary
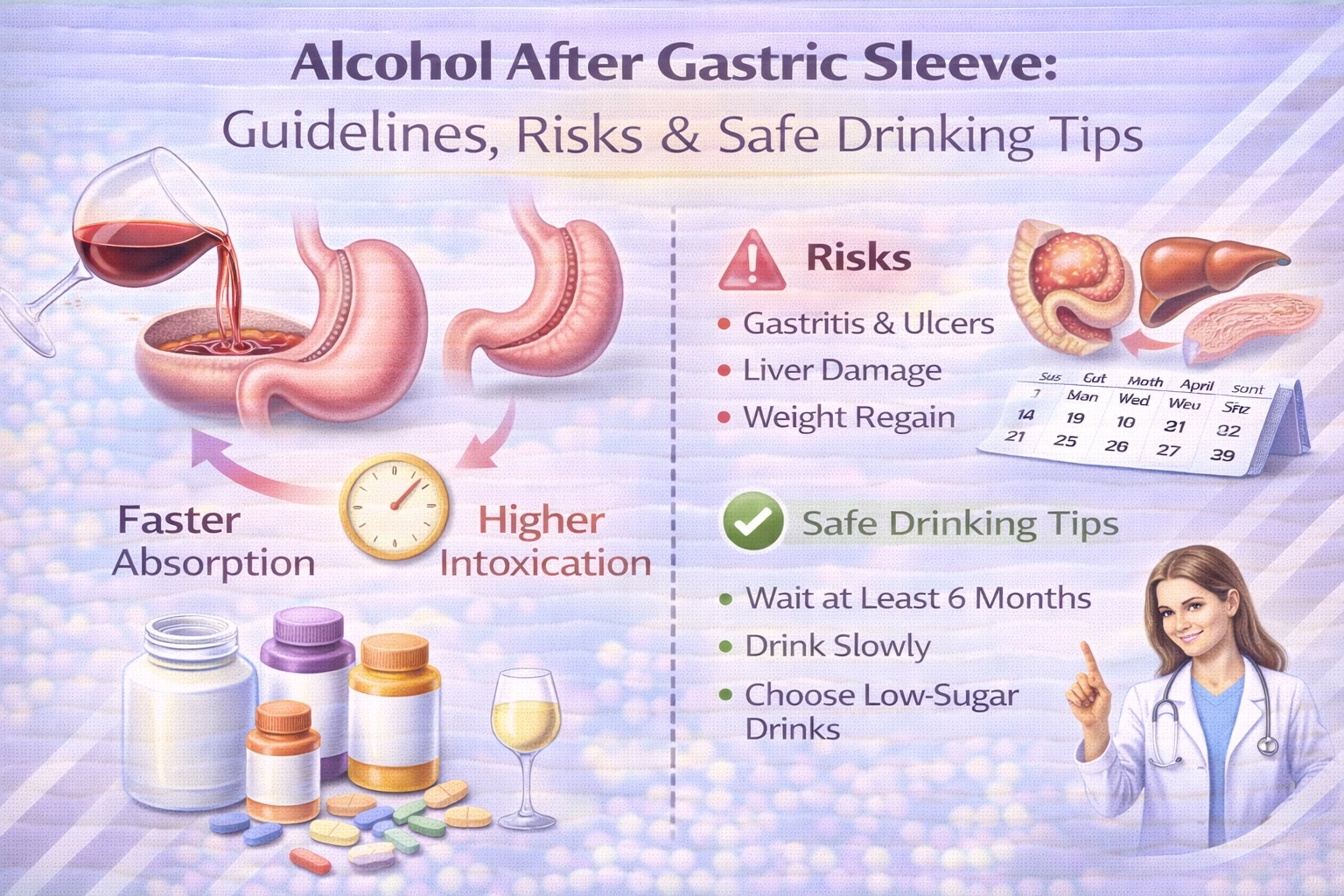
Patients should avoid alcohol for at least 6-12 months after gastric sleeve surgery, as the procedure dramatically alters how the body absorbs and metabolizes alcohol, causing faster intoxication and increased health risks.
According to research published in Surgery for Obesity and Related Diseases, blood alcohol levels peak within 5-9 minutes after drinking post-surgery compared to 25 minutes pre-surgery, with levels reaching nearly double the concentration.
This guide covers why alcohol affects you differently after gastric sleeve, the specific risks, recommended waiting periods, safe drinking guidelines, and warning signs of alcohol use disorder.
Why Trust This Guide
This guide draws from peer-reviewed research in JAMA and Surgery for Obesity and Related Diseases, plus ASMBS/IFSO clinical guidelines, reviewed by Carely Clinic’s bariatric team.
Carely Clinic’s bariatric team has reviewed these recommendations to ensure patients receive accurate, evidence-based guidance for navigating alcohol consumption safely after weight loss surgery.
How Gastric Sleeve Changes Alcohol Metabolism
Gastric sleeve surgery removes approximately 75-80% of the stomach, fundamentally altering how your body processes alcohol by reducing first-pass metabolism and accelerating absorption into the bloodstream.
Before surgery, alcohol passes through the full stomach where an enzyme called alcohol dehydrogenase begins breaking it down before it reaches the small intestine and bloodstream. This process typically takes about 25 minutes for blood alcohol levels to peak after consuming a drink. The stomach essentially acts as a buffer, slowing alcohol absorption and allowing your body time to metabolize it.
After gastric sleeve surgery, this buffer essentially disappears. Research published in Surgery for Obesity and Related Diseases (2018) found that blood alcohol levels in sleeve gastrectomy patients peaked within 9 minutes of finishing a drink, compared to 26 minutes in non-surgery controls. Perhaps more concerning, peak blood alcohol concentrations reached approximately 1.1 g/L in post-surgery patients versus 0.6 g/L in controls—nearly double the level from the same amount of alcohol.
Why This Happens
Several anatomical and physiological changes contribute to altered alcohol metabolism after gastric sleeve:
Reduced stomach volume: With only 20-25% of your original stomach remaining, there is significantly less surface area containing alcohol dehydrogenase, the enzyme responsible for initial alcohol breakdown.
Faster gastric emptying: The smaller stomach empties liquids rapidly into the small intestine, where 80% of alcohol absorption occurs. This accelerated transit means alcohol enters your bloodstream faster and in higher concentrations.
Reduced food buffering: Post-surgery dietary restrictions and smaller meal sizes mean you’re often drinking on a relatively empty stomach, further speeding absorption.
Weight loss impact: As you lose weight, your body composition changes. Less body mass means less volume for alcohol to distribute through, resulting in higher blood alcohol concentrations from the same amount.
Expert Insight
“After gastric sleeve surgery, if a woman has a couple of drinks, she could be exposing her brain to blood alcohol levels that are achieved in a woman without surgery when she consumes four or five drinks.”
— M. Yanina Pepino, PhD, University of Illinois, Surgery for Obesity and Related Diseases (2018)
How Long Should You Wait to Drink Alcohol?
Most bariatric surgeons recommend waiting at least 6-12 months after gastric sleeve surgery before consuming any alcohol, with many experts preferring patients wait the full year or longer.
This waiting period isn’t arbitrary—it serves several critical purposes for your recovery and long-term success:
First 6 Months: Critical Healing Phase
During the initial post-operative period, your stomach is healing from major surgery. The staple line needs time to fully recover, and any alcohol consumption during this phase could irritate the healing tissue, increase inflammation, and potentially compromise surgical outcomes. Alcohol is a known gastric irritant that can damage the stomach lining even in healthy individuals.
Additionally, the first 6 months represent your most rapid weight loss phase. Alcohol provides 7 calories per gram—nearly twice the caloric density of protein or carbohydrates—while offering zero nutritional value. Consuming these “empty calories” during the critical weight loss window can significantly undermine your results.
Months 6-12: Continued Caution
While some surgeons may permit occasional alcohol after 6 months, most recommend waiting the full year. During this period, your body is still adapting to new eating patterns, your sensitivity to alcohol remains extremely high, and you’re establishing lifelong habits that will determine your long-term success.
After 12 Months: Proceed With Extreme Caution
Even after the one-year mark, your relationship with alcohol has permanently changed. You will never process alcohol the way you did before surgery. One drink may affect you like 2-4 drinks did previously, and this increased sensitivity persists indefinitely.
Specific Risks of Drinking After Surgery
Drinking alcohol after gastric sleeve carries several serious health risks that every patient must understand before making decisions about consumption.
Rapid Intoxication
The most immediate concern is how quickly alcohol affects you after surgery. What previously took several drinks to achieve now happens with just one drink—or even a few sips in the early post-operative period. This rapid intoxication increases the risk of accidents, impaired judgment, and alcohol poisoning.
Research shows that patients often underestimate how intoxicated they’ve become because the effects hit so quickly. Breathalyzer readings may also underestimate actual blood alcohol levels by up to 27% in bariatric patients, according to University of Illinois research.
Hypoglycemia (Low Blood Sugar)
Extensive weight loss and reduced carbohydrate intake after gastric sleeve naturally lower glycogen stores in your body. Alcohol consumption further depletes these glycogen reserves, causing blood sugar levels to drop dangerously.
Symptoms of hypoglycemia include dizziness, confusion, weakness, poor coordination, slurred speech, and in severe cases, loss of consciousness. This risk is particularly dangerous because hypoglycemia symptoms mimic intoxication—you or others might assume you’ve simply had too much to drink when you actually need medical intervention.
Increased Ulcer Risk
Alcohol is acidic and irritates the stomach lining. After gastric sleeve, your smaller stomach is more vulnerable to ulcer formation. The combination of reduced protective mucosa and concentrated alcohol exposure significantly increases your risk of developing painful and potentially dangerous stomach ulcers.
Weight Loss Sabotage
Alcohol undermines weight loss through multiple mechanisms:
- Empty calories: A single glass of wine contains 120-150 calories with no nutritional value
- Impaired fat burning: Your liver prioritizes metabolizing alcohol over burning fat
- Lowered inhibitions: Alcohol impairs judgment, making it easier to overeat or choose unhealthy foods
- Nutrient interference: Alcohol blocks absorption of essential vitamins including B12, folate, and thiamine—nutrients already at risk after bariatric surgery
Liver Damage
Post-bariatric surgery patients face elevated risk of alcohol-related liver disease. A 2024 study in the World Journal of Gastrointestinal Surgery found that bariatric surgery patients have increased vulnerability to alcohol-associated liver disease, with some developing cirrhosis faster than non-surgical patients who consume similar amounts.
Stomach Stretching
Binge drinking or excessive alcohol consumption can stretch your stomach pouch, potentially compromising the restriction that makes gastric sleeve effective. This can lead to reduced weight loss or weight regain over time.
Alcohol Use Disorder After Bariatric Surgery
Bariatric surgery patients face elevated alcohol use disorder risk, with 7-33% developing problematic drinking patterns and peak onset occurring around 2 years post-surgery according to research.
Research consistently shows that bariatric surgery patients face elevated risk of developing alcohol use disorder (AUD), making awareness and prevention crucial components of post-operative care.
The Statistics
According to the landmark LABS-2 study published in JAMA (2012), the prevalence of AUD symptoms among gastric bypass patients increased significantly after the second post-operative year. While gastric sleeve appears to carry somewhat lower risk than gastric bypass, the concern remains substantial:
- Approximately 7-10% of bariatric surgery patients develop new problematic alcohol use post-surgery
- AUD prevalence increases from 7% pre-surgery to 16% at 7 years post-surgery in some studies
- Peak onset typically occurs 2 years after surgery
- Up to 33% of bariatric patients may develop AUD at some point in their lifetime
Risk Factors
Certain patients face higher risk of developing alcohol problems after surgery:
- Pre-operative regular alcohol use (2+ drinks per week)
- History of alcohol use disorder (even if in remission)
- Male gender
- Younger age
- Smoking
- Lower sense of social belonging
- History of recreational drug use
Why This Happens
Several mechanisms may explain increased AUD risk after bariatric surgery:
Altered reward pathways: The same neurological changes that reduce food cravings may increase the rewarding effects of alcohol, making it feel more pleasurable.
Heightened sensitivity: Because small amounts produce strong effects, the brain may develop associations between drinking and powerful rewards more quickly.
Enhanced absorption: The rapid, intense alcohol exposure after surgery may create a drug-like “rush” that reinforces addictive patterns.
Psychological factors: Some patients who previously used food for emotional coping may transfer this behavior to alcohol.
Expert Insight
“Patients who undergo bariatric surgery are at increased risk for alcohol use disorders. The risk was found to not be significantly increased in the first 2 years postoperatively but increasing after this period.”
— Annals of Translational Medicine (2018)
Safe Drinking Guidelines If You Choose to Drink
After 12 months with medical clearance, always eat first, start with 2-3 sips, limit to one drink maximum, never drive, and monitor for hypoglycemia symptoms.
If you’ve reached the 12-month mark, received clearance from your bariatric team, and choose to drink alcohol occasionally, following these guidelines can help minimize risks.
Essential Safety Rules
Always eat first: Never drink on an empty stomach. Having food in your system slows alcohol absorption somewhat, though your tolerance will still be dramatically lower than before surgery.
Start extremely small: Your first attempt at alcohol post-surgery should be no more than 2-3 sips. Wait at least 30 minutes to assess the effects before consuming any more.
One drink maximum: Even after a year, consider one drink your absolute maximum. Remember that one drink may feel like 2-4 drinks did before surgery.
Allow hours between drinks: If attending an event where you plan to have more than one drink over several hours, space them far apart—at least 2-3 hours between each drink.
Never drive: Your judgment about impairment may be compromised. Plan for alternative transportation before any drinking.
Drink with a trusted companion: Have someone with you who knows about your surgery and can recognize if you’re becoming intoxicated or unwell.
Stay hydrated: Alternate each alcoholic drink with water. Alcohol is dehydrating, which is particularly dangerous after bariatric surgery when maintaining hydration is already challenging.
Monitor for hypoglycemia: Know the symptoms of low blood sugar and keep glucose tablets or a sugary snack available in case you experience dizziness, confusion, or weakness.
When to Avoid Alcohol Entirely
Some situations warrant complete abstinence:
- You have any history of alcohol use disorder
- You’re taking medications that interact with alcohol
- You’re experiencing dumping syndrome or other GI issues
- You haven’t reached your weight loss goals
- You notice yourself wanting to drink more frequently
- You’re using alcohol to cope with emotions
Best and Worst Alcoholic Beverages After Gastric Sleeve
Dry wine and spirits with non-carbonated mixers are better tolerated, while beer, champagne, sweet cocktails, and creamy liqueurs should be avoided due to carbonation and sugar.
Not all alcoholic beverages affect post-surgery patients equally. If you choose to drink, selecting wisely can reduce (though not eliminate) certain risks.
Better Options (Used Sparingly)
Dry wine: A 5-ounce glass of dry red or white wine contains approximately 120-130 calories and no carbonation. Dry wines have lower sugar content than sweet varieties.
Spirits with non-carbonated mixers: Vodka, gin, or tequila mixed with water, a splash of citrus, or a zero-calorie, non-carbonated mixer. Avoid fruit juices and sodas.
Light beer (non-carbonated alternatives): While regular beer is problematic due to carbonation, some patients tolerate non-carbonated low-calorie options.
Beverages to Avoid
Beer and carbonated alcoholic drinks: Carbonation causes gas, bloating, discomfort, and can stretch your stomach pouch. This includes champagne, sparkling wines, hard seltzers, and beer.
Sweet cocktails and mixers: Margaritas, daiquiris, and drinks made with juice, soda, or simple syrup are loaded with sugar and calories that can trigger dumping syndrome and sabotage weight loss.
Creamy liqueurs: Bailey’s, Kahlúa, and similar cream-based drinks are high in sugar and fat.
High-proof spirits (shots): Concentrated alcohol hits your bloodstream even faster and makes it harder to control intake.
Warning Signs to Watch For
Watch for physical signs (severe hangovers, hypoglycemia, stomach pain) and behavioral patterns (drinking alone, using alcohol to cope, drinking more than planned) that indicate problematic use.
Recognizing problematic drinking patterns early allows for intervention before alcohol use disorder develops.
Physical Warning Signs
- Getting drunk from very small amounts
- Severe hangovers from minimal drinking
- Experiencing hypoglycemia after drinking
- Nausea or vomiting when drinking
- Stomach pain or discomfort
- Weight loss stalling or weight regain
Behavioral Warning Signs
- Thinking about alcohol frequently
- Drinking alone or hiding alcohol use
- Using alcohol to cope with emotions
- Drinking more than you planned
- Needing more alcohol to achieve the same effect
- Continuing to drink despite negative consequences
- Feeling guilty about drinking
When to Seek Help
If you recognize any of these patterns, contact your bariatric team immediately. Early intervention significantly improves outcomes. Resources include:
- Your bariatric surgeon and care team
- Mental health professionals specializing in addiction
- Support groups for bariatric patients
- Alcohol Use Disorder treatment programs
How This Applies in Turkey
International guidelines from the ASMBS and IFSO regarding alcohol and bariatric surgery apply at Turkey’s JCI-accredited medical facilities, with Turkish hospitals following identical clinical protocols and safety standards as American and European institutions.
The key advantage for international patients is the comprehensive aftercare included in Turkish bariatric packages. Gastric sleeve surgery in Turkey costs €3,500-€5,500 all-inclusive, compared to $15,000-$25,000 in the USA and £10,000-£15,000 in the UK—representing savings of 60-75% while maintaining identical medical standards.
At Carely Clinic in Istanbul, gastric sleeve surgery is performed by board-certified bariatric surgeons at JCI-accredited partner hospitals. Packages include pre-operative consultations, surgery, hospital stay, medications, and comprehensive aftercare guidance—including detailed counseling on alcohol and lifestyle modifications. Learn more about Gastric Sleeve Surgery at Carely Clinic.
Summary Table
| Topic | Guideline | Key Details |
|---|---|---|
| Minimum Waiting Period | 6-12 months | Most surgeons recommend waiting the full year; never drink before 6 months |
| Blood Alcohol Peak Time | 5-9 minutes post-surgery | Compared to 25 minutes pre-surgery; nearly 3x faster absorption |
| Peak Blood Alcohol Level | Nearly 2x higher | Same amount of alcohol produces double the blood concentration |
| Alcohol Use Disorder Risk | 7-33% of patients | Peak onset at 2 years post-surgery; higher with gastric bypass than sleeve |
| Beverages to Avoid | Carbonated, sugary drinks | Beer, champagne, seltzers, cocktails with juice/soda, cream liqueurs |
| Safer Options | Dry wine, spirits with water | Still only in extreme moderation; one drink maximum recommended |
| Key Risks | Multiple serious concerns | Rapid intoxication, hypoglycemia, ulcers, liver damage, weight regain |
Frequently Asked Questions
Can I ever drink alcohol again after gastric sleeve surgery?
Yes, after 6-12 months with medical clearance. However, you’ll remain permanently more sensitive, requiring extreme moderation and safety precautions for life.
What happens if I drink alcohol 3 weeks after gastric sleeve?
Drinking 3 weeks post-surgery risks severe nausea, rapid intoxication, hypoglycemia, and compromised healing. Your stomach is still vulnerable and alcohol sensitivity is at peak levels.
Why do I get drunk so fast after gastric sleeve?
Your smaller stomach rapidly empties alcohol into your intestine with less breakdown enzyme. Blood alcohol peaks in 5-9 minutes at nearly double the concentration compared to pre-surgery.
Does gastric sleeve increase alcoholism risk?
Yes. Research shows 7-33% of patients develop problematic drinking, with peak onset around 2 years post-surgery. Risk factors include pre-surgical alcohol use, younger age, and smoking.
Is wine or beer safer after gastric sleeve?
Dry wine is better tolerated than beer. Beer’s carbonation causes bloating and stomach stretching. However, neither is truly “safe”—both require extreme moderation and medical clearance.
How much alcohol is one drink after gastric sleeve?
One standard drink measures the same (5oz wine, 12oz beer, 1.5oz spirits), but the effect feels like 2-4 pre-surgery drinks. Start with 2-3 sips first.
Can alcohol cause weight regain after gastric sleeve?
Yes. Alcohol provides empty calories (7 per gram), impairs fat burning, lowers inhibitions leading to poor food choices, and can stretch your stomach with excessive consumption.
What are signs of hypoglycemia after drinking?
Symptoms include dizziness, confusion, weakness, shakiness, sweating, rapid heartbeat, slurred speech, and loss of consciousness. These mimic intoxication, so monitor carefully and keep glucose tablets available.
Should I eat before drinking alcohol after gastric sleeve?
Yes, always eat before drinking to slow absorption somewhat. Choose protein-rich foods over carbohydrates. Never drink on an empty stomach as this significantly increases risks.
When should I seek help for alcohol use after gastric sleeve?
Contact your bariatric team if you’re drinking more than planned, hiding use, drinking to cope emotionally, or if others express concern. Early intervention improves outcomes significantly.
Conclusion
Alcohol after gastric sleeve surgery carries significant risks that every patient must understand. The surgery fundamentally changes how your body processes alcohol—causing faster absorption, higher blood alcohol concentrations, and increased sensitivity that persists indefinitely.
The safest approach is to avoid alcohol entirely during the first 6-12 months, and to drink only in extreme moderation thereafter if you choose to resume at all. Patients with any history of alcohol use disorder should consider permanent abstinence given the elevated risk of relapse after bariatric surgery.
If you do choose to drink after the recommended waiting period, follow strict safety guidelines: always eat first, start with tiny amounts, never drive, and remain vigilant for warning signs of problematic use. Your long-term health and weight loss success depend on making informed, careful choices.
Disclaimer: This guide provides general information based on current medical guidelines and research. Individual requirements and outcomes vary. Consult with your bariatric surgeon and healthcare team for personalized guidance regarding alcohol consumption after your surgery.
For questions about gastric sleeve surgery and comprehensive aftercare support, contact Carely Clinic to schedule a consultation with our experienced bariatric team.