Quick Summary
Gastric sleeve bougie size directly impacts weight loss and complications, with 33-36 French (Fr) offering optimal balance—smaller bougies produce 6.7% greater weight loss but 2.14x higher stricture risk.
According to 2024 network meta-analysis of 13,450 patients, larger bougies (≥40 Fr) reduce leak rates from 2.67% to 0.92%.
This guide covers optimal bougie sizes, complication rates, weight loss differences, surgeon selection criteria, and what to ask your bariatric surgeon.
Why Trust This Guide
This guide synthesizes evidence from multiple peer-reviewed sources including network meta-analyses published in Obesity Surgery, the International Sleeve Gastrectomy Expert Panel Consensus Statement based on over 12,000 cases, registry data from the Scandinavian Obesity Surgery Registry, and clinical studies published in Surgery for Obesity and Related Diseases.
All statistics and recommendations reference current bariatric surgery guidelines and are presented for educational purposes to help patients understand this important surgical variable.
What Is a Bougie in Gastric Sleeve Surgery?
A bougie is a flexible calibration tube inserted through the patient’s mouth to guide stomach resection during gastric sleeve surgery, with sizes ranging from 32-50 French (Fr) determining the final sleeve diameter.
The bougie serves as a template around which the surgeon staples and removes approximately 75-80% of the stomach. Bougies are measured using the French scale (abbreviated Fr or F), where each French unit equals 0.333 millimeters (1/3 mm). To calculate the diameter in millimeters, simply divide the French size by 3. For example, a 36 Fr bougie has a diameter of 12 mm, while a 40 Fr bougie measures approximately 13.3 mm—roughly half an inch.
The bougie performs several critical functions during surgery. It ensures consistent sleeve diameter throughout the procedure, helps the surgeon avoid stapling too close to the stomach wall, provides a reference point for removing the appropriate amount of stomach tissue, and ultimately determines how much food the new stomach can hold. A smaller bougie creates a narrower, more restrictive sleeve, while a larger bougie leaves a wider stomach tube with greater capacity.
Standard bougie sizes used in gastric sleeve surgery range from 32 Fr to 50 Fr, though most bariatric surgeons favor sizes between 34 Fr and 40 Fr for routine procedures. The selection depends on multiple factors including the patient’s BMI, anatomy, comorbidities, and the surgeon’s training and experience.
Common Bougie Sizes and Their Diameters
| French Size (Fr) | Diameter (mm) | Diameter (inches) |
|---|---|---|
| 32 Fr | 10.7 mm | 0.42″ |
| 34 Fr | 11.3 mm | 0.45″ |
| 36 Fr | 12.0 mm | 0.47″ |
| 38 Fr | 12.7 mm | 0.50″ |
| 40 Fr | 13.3 mm | 0.52″ |
| 50 Fr | 16.7 mm | 0.66″ |
Understanding these measurements helps contextualize the relatively small differences between bougie sizes. The difference between a 32 Fr and 40 Fr bougie is approximately 2.6 mm—yet this seemingly minor variation produces measurable differences in outcomes across large patient populations.
How Bougie Size Affects Weight Loss
Smaller bougie sizes (32-36 Fr) produce approximately 6.7% greater excess weight loss compared to larger sizes, according to a 2024 network meta-analysis of 35 studies involving 13,450 patients published in Obesity Surgery. However, this difference, while statistically significant, may not be clinically meaningful for all patients.
The relationship between bougie size and weight loss follows logical principles. A narrower sleeve restricts food intake more aggressively, forcing patients to eat smaller portions and feel full faster. The fundus—the stretchy upper portion of the stomach that produces the hunger hormone ghrelin—is more completely removed with smaller bougies, potentially reducing appetite signals more effectively.
Research from the Scandinavian Obesity Surgery Registry found that patients receiving sleeves calibrated with 30-32 Fr bougies lost approximately 3.7% more total body weight at 2 years compared to those with 35-36 Fr bougies. When combined with closer antral resection (starting the staple line 1-4 cm from the pylorus), this difference became more pronounced.
Despite these findings, the weight loss advantage of smaller bougies diminishes over time. One prospective study comparing 32 Fr versus 36 Fr bougies found nearly identical one-year excess weight loss: 73.0% versus 71.1%, a difference that was not statistically significant (p = 0.73). The BOUST trial protocol notes that concerns about larger bougies leading to reduced weight loss “appear to be unfounded in the literature.”
The International Sleeve Gastrectomy Expert Panel Consensus Statement, based on experience with over 12,000 cases, recommends 32-36 Fr bougies for most patients, acknowledging that this range provides excellent weight loss results while managing complication risk. The Fifth International Consensus Conference reported a median recommended bougie size of 36 Fr among expert surgeons.
Bougie Size and Complication Rates
Bougie size significantly influences two major complications: staple line leaks and sleeve strictures. The relationship follows opposite patterns—smaller bougies increase stricture risk while larger bougies reduce leak rates.
Staple Line Leaks
A systematic review analyzing 32 publications with 4,999 patients found that bougies ≥40 Fr produced a leak rate of only 0.92%, compared to 2.67% with smaller bougies—a statistically significant difference (p < 0.05). The 2024 meta-analysis in Obesity Surgery confirmed this pattern, noting that larger bougies create less tension on the staple line and maintain better blood flow to the tissue edges.
Leaks typically occur at the gastroesophageal junction, where the stomach’s blood supply depends heavily on vessels that may be compromised during fundus resection. Smaller bougies create higher intraluminal pressure and tighter sleeves, increasing mechanical stress on staple lines. The StatPearls medical reference notes that “a larger bougie size will decrease the incidence of leaks in sleeve gastrectomy patients.”
Strictures and Stenosis
Conversely, smaller bougies carry higher stricture risk. The 2024 network meta-analysis found bougie sizes 32-36 Fr produced an odds ratio of 2.14 for strictures compared to larger sizes (95% CI: 1.36-3.37, p = 0.001). Strictures occur when the sleeve narrows excessively, particularly at the incisura angularis (the natural bend in the stomach), causing difficulty swallowing, nausea, and vomiting.
The Scandinavian Obesity Surgery Registry reported a symptomatic obstruction rate of 0.6% overall, with 61% of cases occurring at the incisura angularis. Notably, their data showed that narrow bougie sizes (30-32 Fr) were not associated with increased early or late complications in their large cohort, though individual center variation exists.
Stricture symptoms typically develop within the first few months after surgery and may include persistent nausea and vomiting, difficulty tolerating solid foods, progressive food intolerance, regurgitation, and upper abdominal discomfort after eating. Treatment usually involves endoscopic balloon dilation, which successfully resolves most strictures in one or two sessions. Severe or refractory cases may require surgical revision or conversion to gastric bypass.
Gastroesophageal Reflux
Smaller bougies also correlate with increased gastroesophageal reflux disease (GERD). The 2024 meta-analysis reported an odds ratio of 1.76 for GERD with 32-36 Fr bougies compared to larger sizes (95% CI: 1.12-2.78, p = 0.015). The tighter sleeve creates higher pressure, promoting reflux of stomach contents into the esophagus.
What Size Bougie Do Surgeons Use?
Most bariatric surgeons worldwide use 34-40 Fr bougies, with 36 Fr most common among high-volume experts per International Sleeve Gastrectomy Expert Panel (87% consensus for 32-36 Fr range).
The International Sleeve Gastrectomy Expert Panel expressed concerns that sizes below 32 Fr “might increase complications significantly” and sizes above 36 Fr “could lead to lack of weight loss.”
Survey data from the Fifth International Consensus Conference (2014) showed that expert surgeons—defined as those who had performed over 1,000 sleeve gastrectomies—demonstrated significantly different preferences than general bariatric surgeons. Experts were more likely to agree that “the smaller the bougie size and tighter the sleeve, the higher the incidence of leaks” (78.8% vs 65.2%, p = 0.006).
The StatPearls medical reference, maintained by the National Center for Biotechnology Information, recommends using a 32 to 40 Fr bougie and notes that the Fifth International Consensus Conference suggested a “large bougie should be used (median was 36 French).”
Regional variation exists. Some Mexican and Turkish centers routinely use 34 Fr bougies, while certain U.S. academic centers prefer 40 Fr or larger. These differences reflect institutional protocols, training traditions, and varying emphasis on maximizing weight loss versus minimizing complications.
Expert Insight
“The present consensus report represents the best practice guidelines for the performance of LSG, with recommendations in patient selection, contraindications, surgical technique, and the prevention and management of complications. This report supports a first effort toward the standardization of techniques and adoption of working recommendations formulated according to expert experience.”
— International Sleeve Gastrectomy Expert Panel Consensus Statement (2012), based on >12,000 cases
Individualized Selection Factors
Experienced surgeons individualize bougie selection based on multiple patient factors:
Higher BMI patients (BMI >50): May receive larger bougies (38-40 Fr) to reduce complication risk, as they typically achieve substantial weight loss regardless of sleeve diameter.
Lower BMI patients (BMI 35-40): May benefit from smaller bougies (32-36 Fr) to maximize restriction, as weight loss differences become more clinically relevant.
Patients with GERD history: Often receive larger bougies to minimize reflux worsening, though some surgeons consider GERD a relative contraindication for sleeve gastrectomy.
Anatomical variations: Patients with larger existing stomachs or unusual anatomy may require adjusted bougie sizes.
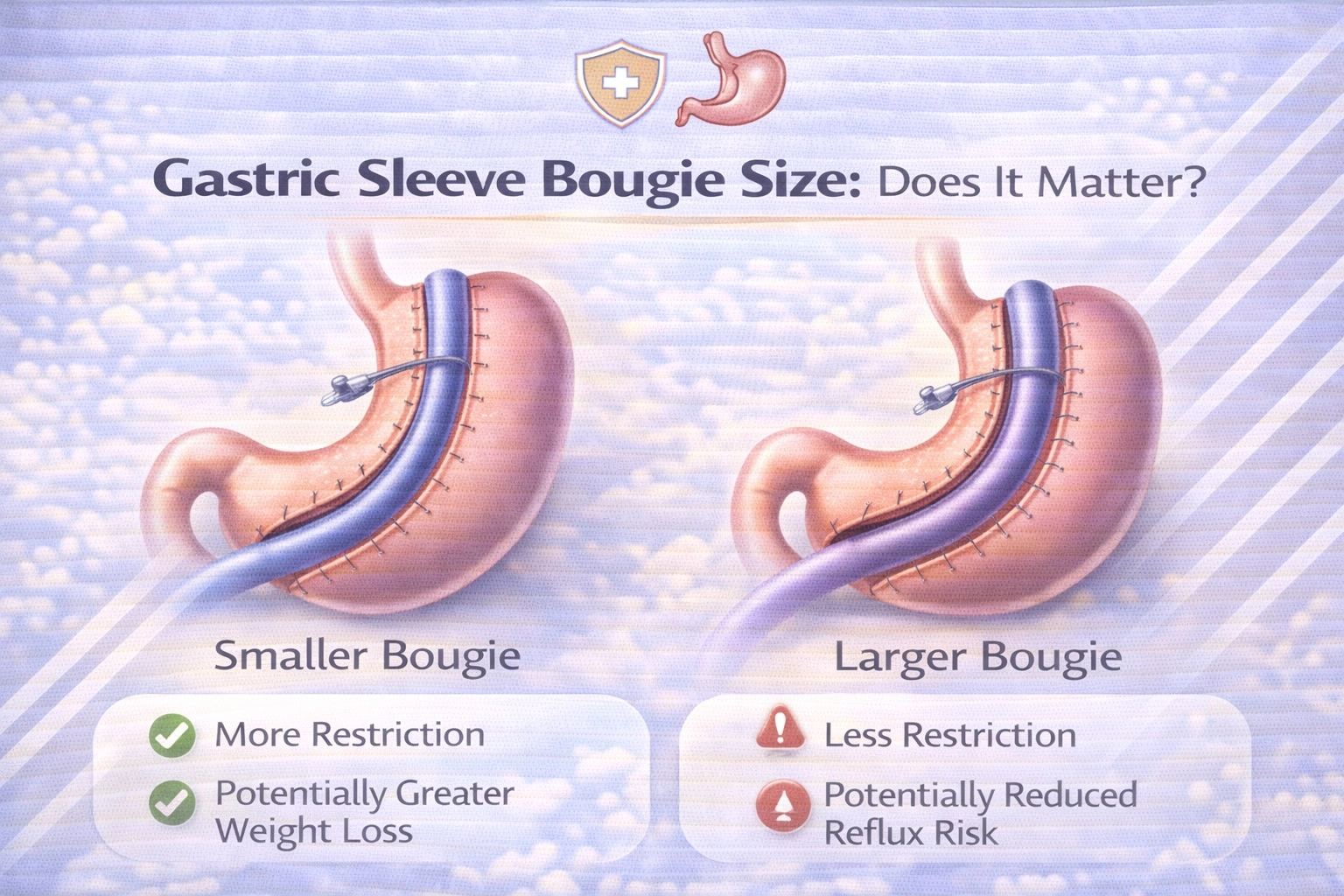
Small vs. Large Bougie: The Trade-offs
Smaller bougies (32-36 Fr) offer 6.7% greater weight loss but carry 2.14x higher stricture risk, while larger bougies (≥40 Fr) reduce leak rates from 2.67% to 0.92%.
Understanding these trade-offs helps patients engage in informed discussions with their surgical teams.
Smaller Bougies (32-36 Fr)
Advantages:
- Greater excess weight loss (approximately 5-7% more)
- Smaller stomach capacity creates stronger restriction
- More complete removal of ghrelin-producing fundus tissue
Disadvantages:
- Higher stricture risk (OR 2.14)
- Increased GERD symptoms (OR 1.76)
- Longer hospital stays in some studies
- More nausea and vomiting in early recovery
- Higher emergency department return rates
Larger Bougies (≥40 Fr)
Advantages:
- Significantly lower leak rate (0.92% vs 2.67%)
- Reduced stricture risk
- Shorter hospital stays
- Better food tolerance in early recovery
- Lower reflux rates
Disadvantages:
- Potentially less weight loss (though difference may not be clinically significant)
- Theoretically greater long-term stretching potential
- May require stronger dietary adherence for optimal results
The “Sweet Spot”
Current evidence suggests mid-range bougie sizes (36-40 Fr) represent the optimal balance for most patients. A 2021 network meta-analysis published in Scientific Reports concluded that “using the M-sized bougie (bougie size between 33 and 36 Fr, including 36 Fr) for intraoperative calibration is an optimal choice to balance the effectiveness and safety during LSG.”
This recommendation recognizes that the modest weight loss advantage of smaller bougies must be weighed against meaningfully higher complication rates, particularly for strictures that may require endoscopic dilation or surgical revision.
Expert Insight
“The calibration bougie size is a critical technical factor that influences outcomes, yet no universal consensus exists regarding optimal sizing. While mid-range bougie sizes (36-40 Fr) may balance weight loss efficacy and safety for many patients, bougie selection should be individualized based on patient characteristics, surgeon experience, and institutional protocols.”
— 2024 Network Meta-Analysis, Obesity Surgery
Does Bougie Size Affect Long-Term Weight Regain?
No, bougie size does not significantly influence long-term weight regain—patient behavior, metabolic adaptation, and lifestyle adherence matter far more than initial sleeve diameter.
Research consistently shows this pattern across multiple studies. The pattern of weight change after sleeve gastrectomy follows a predictable trajectory regardless of bougie size: patients reach peak weight loss around 18-24 months post-surgery, maintain relative stability for several years, then gradually regain a small amount of weight. Up to 50% of patients may regain approximately 5% of their lost weight over time—a phenomenon related to hormonal adaptation and dietary behaviors rather than sleeve calibration.
Factors That Actually Influence Long-Term Success
While bougie size plays a role in initial restriction, these factors demonstrate greater influence on sustained weight loss:
Dietary adherence: Following post-operative nutrition guidelines, including protein-first eating, avoiding grazing behaviors, and limiting calorie-dense foods, directly correlates with long-term success.
Physical activity: Regular exercise helps maintain muscle mass, boost metabolism, and support psychological well-being during weight maintenance.
Behavioral support: Patients who engage in support groups, counseling, or behavioral therapy show better outcomes at 5+ years.
Metabolic factors: Individual variations in hormonal responses, particularly ghrelin and GLP-1 levels, affect hunger and satiety independent of mechanical restriction.
Comorbidity management: Addressing underlying conditions like depression, sleep disorders, and hormonal imbalances supports sustained weight maintenance.
Concerns that larger bougies lead to sleeve dilation and weight regain have not been substantiated in clinical research. The BOUST trial protocol explicitly notes that “concerns of bariatric surgeons whether the use of a larger bougie could lead to weight regain appear to be unfounded in the literature.”
The Scandinavian Obesity Surgery Registry data found that while combining narrow bougies with closer antral resection produced additional short-term weight loss, long-term outcomes beyond 2 years showed convergence between groups. This suggests that while initial restriction matters for early weight loss, sustained success depends primarily on metabolic and behavioral factors.
How This Applies in Turkey
International IFSO guidelines apply equally at Turkey’s JCI-accredited facilities, with Turkish surgeons using the same 34-36 Fr bougie sizes and evidence-based protocols as American and European institutions.
Turkish hospitals follow identical clinical protocols and safety standards as Western institutions, with surgeon training reflecting the same evidence-based approaches to bougie selection. The key differences for international patients are cost and accessibility. Gastric sleeve surgery in Turkey costs €3,500-€5,500 compared to $15,000-$25,000 in the USA and £9,000-£15,000 in the UK—representing savings of 60-75%. International patients typically complete the entire surgical journey within 5-7 days, compared to months of waiting in countries with insurance-based systems.
Turkish bariatric surgeons commonly use 34-36 Fr bougies, aligning with international expert recommendations. High-volume centers perform hundreds of sleeve gastrectomies annually, maintaining complication rates comparable to or better than Western academic centers. JCI accreditation ensures facilities meet rigorous international standards for patient safety, infection control, and surgical outcomes.
At Carely Clinic in Istanbul, gastric sleeve surgery is performed by board-certified surgeons at JCI-accredited partner hospitals. All-inclusive packages cover hospital stay, surgeon fees, pre-operative testing, post-operative medications, accommodation, and transportation. Surgeons discuss bougie selection during pre-operative consultations, individualizing the approach based on patient characteristics and goals.
Learn more about Gastric Sleeve Surgery at Carely Clinic.
Bougie Size Comparison Summary
| Bougie Size | Diameter (mm) | Weight Loss | Leak Rate | Stricture Risk | Best For |
|---|---|---|---|---|---|
| Small (≤32 Fr) | ≤10.7 | Highest | ~2.67% | Higher (OR 2.14) | Lower BMI patients prioritizing maximum restriction |
| Medium (33-36 Fr) | 11-12 | High | ~1.5-2% | Moderate | Most patients (optimal balance) |
| Large (37-40 Fr) | 12.3-13.3 | Good | ~0.92% | Lower | Higher BMI patients, those with GERD history |
| Extra Large (>40 Fr) | >13.3 | Moderate | <0.92% | Lowest | High-risk patients prioritizing safety |
Data synthesized from 2024 network meta-analysis (Obesity Surgery) and 2013 systematic review (Obes Surg)
Questions to Ask Your Surgeon About Bougie Size
Discussing bougie selection with your surgeon demonstrates informed engagement with your surgical plan. Consider asking these questions during your consultation:
- “What bougie size do you typically use, and why?” This reveals the surgeon’s approach and reasoning.
- “How do you individualize bougie selection for different patients?” Look for thoughtful consideration of patient factors rather than one-size-fits-all approaches.
- “What are your leak and stricture rates?” Complication rates matter more than bougie size alone—an experienced surgeon with excellent outcomes using any standard bougie size is preferable to less experienced surgeons with “optimal” sizes.
- “Given my BMI and health conditions, what size would you recommend for me?” Personalized recommendations indicate patient-centered care.
- “How does bougie size affect my expected weight loss?” This tests whether the surgeon provides balanced, evidence-based information.
Other Surgical Factors That Influence Outcomes
Bougie size is one of several critical variables—staple line reinforcement, pylorus distance, staple height selection, and surgeon volume all significantly impact leak rates and weight loss outcomes.
Understanding these factors provides context for why experienced surgeons may achieve excellent results across different bougie preferences.
Distance from Pylorus
The starting point of the staple line—measured as distance from the pylorus—significantly impacts both weight loss and complications. The Scandinavian Obesity Surgery Registry found that starting the resection 1-4 cm from the pylorus produced greater weight loss than the standard 5 cm distance, but also increased early complication rates. Most expert guidelines recommend beginning the staple line 4-6 cm from the pylorus.
Staple Line Reinforcement
Surgeons may reinforce the staple line using oversewing, buttressing materials (such as bovine pericardium or synthetic strips), or no reinforcement. A 2016 meta-analysis found that staple line reinforcement did not significantly reduce leak rates but did decrease overall complications, including staple line bleeding. The Fifth International Consensus Conference reported that most experts now use some form of reinforcement.
Staple Height Selection
Staple height must match tissue thickness, which varies along the stomach. The antrum (lower stomach) averages 3.1 mm thick, the body 2.4 mm, and the fundus 1.7 mm. Using appropriately sized staples for each region helps ensure proper closure and reduces complication risk. Most surgeons use different staple heights (colors) for different stomach sections.
Surgeon Experience and Volume
Perhaps the most important factor is surgeon experience. High-volume bariatric surgeons—those performing 100+ procedures annually—consistently achieve lower complication rates regardless of specific technical choices. Studies show significant learning curves for sleeve gastrectomy, with outcomes improving substantially after the first 50-100 cases.
Frequently Asked Questions
What is the most commonly used bougie size for gastric sleeve?
The 36 Fr bougie is most commonly used by expert bariatric surgeons worldwide. The International Sleeve Gastrectomy Expert Panel reports 87% consensus for 32-36 Fr bougies, with 36 Fr as the median size among surgeons who performed over 1,000 procedures.
Does a smaller bougie guarantee more weight loss?
No, smaller bougies do not guarantee more weight loss. While 32-36 Fr bougies show 6.7% greater excess weight loss in meta-analyses, one-year outcomes comparing 32 Fr versus 36 Fr showed nearly identical results (73% vs 71% EWL). Long-term success depends primarily on lifestyle adherence.
Why would a surgeon choose a larger bougie?
Surgeons choose larger bougies (≥40 Fr) primarily to reduce leak rates from 2.67% to 0.92%. Larger sizes are preferred for patients with higher surgical risk, GERD history, super-obesity (BMI >50), or anatomical considerations where safety takes priority over maximum restriction.
Can I request a specific bougie size from my surgeon?
Yes, you can discuss bougie size preferences, but the final decision should reflect your surgeon’s clinical judgment. Experienced surgeons consider BMI, anatomy, comorbidities, and surgical risk factors that patients cannot fully evaluate. Trust their expertise while understanding their reasoning.
What is the relationship between bougie size and leak risk?
Larger bougies significantly reduce leak rates to 0.92% compared to 2.67% with smaller bougies. A systematic review of 4,999 patients found bougies ≥40 Fr produced this dramatic reduction (p < 0.05) because narrower sleeves generate higher pressure on staple lines.
How is bougie size measured?
Bougies use the French scale where 1 French equals 0.333 mm. Divide the French number by 3 to get millimeters—for example, a 36 Fr bougie measures 12 mm (approximately 0.5 inches) in diameter.
Does bougie size affect gastric sleeve stricture risk?
Yes, smaller bougie sizes (32-36 Fr) carry significantly higher stricture risk with an odds ratio of 2.14. Strictures cause narrowing at the incisura angularis, leading to difficulty swallowing, nausea, vomiting, and potential need for endoscopic dilation treatment.
Will my sleeve stretch more with a larger bougie?
No, research does not support this concern—long-term weight regain patterns are similar regardless of initial bougie size. The BOUST trial protocol confirms that “concerns about larger bougies leading to weight regain appear to be unfounded in the literature.”
What bougie size do Turkish surgeons typically use?
Turkish bariatric surgeons commonly use 34-36 Fr bougies, consistent with international expert recommendations. High-volume Turkish centers follow the same evidence-based ASMBS and IFSO guidelines as American and European institutions, with individualized selection based on patient characteristics.
Is there an “ideal” bougie size for everyone?
No universal ideal exists—current evidence suggests 33-40 Fr provides an appropriate range with 36 Fr as a reasonable default. The optimal size varies based on individual patient factors including BMI, anatomy, comorbidities, surgeon experience, and institutional protocols.
How much does bougie size affect final stomach capacity?
Standard bougie sizes (32-40 Fr) create sleeves holding 100-150 mL initially, expanding slightly over time. The capacity difference between 32 Fr and 40 Fr sleeves is modest—both create significant restriction compared to the original 1,000-1,500 mL stomach capacity.
Should I be worried if my surgeon uses a 40 Fr bougie?
No, a 40 Fr bougie is within the standard expert-recommended range and produces excellent outcomes. Large studies show 65-70% excess weight loss with 40 Fr bougies plus significantly lower leak rates (0.92%). Surgeon experience and technique matter more than bougie size alone.
Conclusion
Gastric sleeve bougie size represents one of many technical variables that influence surgical outcomes—but it is not the only or even the most important factor determining your success. The evidence shows that mid-range bougie sizes (33-40 Fr) provide excellent weight loss results while maintaining acceptable complication rates, with 36 Fr emerging as the most commonly recommended size among expert bariatric surgeons worldwide.
The key findings from current research are clear: smaller bougies (≤36 Fr) produce modestly greater short-term weight loss but carry higher stricture and reflux risk, while larger bougies (≥40 Fr) significantly reduce leak rates without meaningfully compromising weight loss outcomes. Most importantly, long-term success depends primarily on lifestyle adherence, dietary habits, and psychological readiness for permanent change—not bougie calibration alone.
When evaluating bariatric surgery options, focus on surgeon experience, hospital accreditation, comprehensive pre- and post-operative support, and realistic outcome expectations rather than fixating on specific bougie sizes. An experienced surgeon using any standard bougie size (32-40 Fr) with excellent technique will produce better outcomes than an inexperienced surgeon with the “optimal” size.
Individual requirements and outcomes vary. This guide provides general information based on international guidelines and peer-reviewed research. Consult qualified medical professionals for personalized advice regarding your bariatric surgery options.
Ready to learn more about your gastric sleeve surgery options? Contact Carely Clinic for a free consultation with our experienced bariatric team.